To Buy Pregabalin Online Visit Our Pharmacy ↓
 Pregabalin Vs Gabapentin: Key Differences Explained
Pregabalin Vs Gabapentin: Key Differences Explained
Mechanisms Unraveled What Truly Sets Them Apart
They both quiet neuronal hyperexcitability by targeting the alpha2-delta subunit of voltage-gated calcium channels, reducing calcium influx and dampening release of excitatory neurotransmitters such as glutamate and substance P. However, pregabalin binds with greater affinity and reaches the central nervous system faster, producing more predictable effects.
Gabapentin relies on a saturable L-amino acid transporter for gut absorption, so its bioavailability falls at higher doses and onset can be variable between patients. Pregabalin follows linear uptake, giving steadier plasma levels and simpler dose titration.
Clinically this means similar therapeutic goals but different practical choices: gabapentin may require flexible dosing and patience with titration, while pregabalin often yields quicker, more consistent responses, which can influence selection based on symptom urgency, comorbidity and tolerability. Prescribers weigh cost, side effects and abuse risk when choosing between them. Patient preference also matters, and real-world experience.
| Feature | Gabapentin | Pregabalin |
|---|---|---|
| Binding affinity | Lower | Higher |
| Absorption | Saturable, dose-dependent | Linear, predictable |
Pharmacokinetics and Dosing Absorption Half Life Differences

Think of two travelers reaching relief by different routes: pregabalin is absorbed rapidly with predictable, linear kinetics and high bioavailability, so it acts sooner and allows straightforward dosing.
Their half‑lives are short, so dosing frequency matters: pregabalin’s more predictable exposure often lets clinicians use twice‑daily schedules, whereas gabapentin commonly requires three daily doses because absorption saturates at higher amounts. Both are cleared by the kidneys, necessitating dose reductions in renal impairment, and gabapentin’s variable uptake can complicate titration compared with pregabalin’s steadier profile. Many patients notice onset differences in practice.
Approved Indications and Surprising Off Label Uses
Clinicians often reach for gabapentinoids when conventional treatments fail; pregabalin emerged with clear regulatory approvals for several neuropathic and pain-related conditions.
It is licensed for diabetic peripheral neuropathy, postherpetic neuralgia, adjunctive therapy for focal seizures and, in many countries, for fibromyalgia and generalized anxiety disorder.
Beyond labels, prescribers try these agents off-label for restless legs, chronic cough, bipolar spectrum symptoms and refractory insomnia—sometimes with meaningful symptom relief but limited trial evidence.
Patients should discuss realistic expectations, adverse effects and tapering plans with clinicians, because approved uses, off-label experimentation and individual risk-benefit decisions demand careful monitoring. Dose adjustments for renal impairment, potential interactions, pregnancy considerations and monitoring for misuse are important points to cover during follow-up.
Side Effects Showdown Tolerability and Common Reactions

Patients often describe the initial days on pregabalin or gabapentin as a fog: dizziness, somnolence and blurred vision can dull edges of daily life. Less common reactions include weight gain, peripheral edema and dry mouth; many settle with dose adjustment. Clinicians aim for the lowest effective dose to balance symptom relief and cognitive side effects.
Gastrointestinal upset and coordination problems are possible, especially when combined with opioids or alcohol, increasing fall risk. Rare but serious events—hypersensitivity reactions, mood changes and respiratory depression in vulnerable patients—require prompt attention. Regular review, patient education and gradual tapering help optimize tolerability and safety. Monitoring kidney function and adjusting for renal impairment further reduces adverse outcome risk in susceptible patients.
Abuse Potential Dependence Risk and Safety Alerts
Clinicians increasingly monitor real-world misuse reports. Pregabalin’s rapid onset and rewarding sensations in some patients have prompted warnings, encouraging prescribers to screen risk factors before initiating therapy and counsel proactively.
Dependence risk rises with long-term use; abrupt cessation causes withdrawal symptoms including anxiety, insomnia and dizziness. Gradual tapering plans and patient education reduce severity and recurrence of symptoms in practice.
Regulatory safety alerts have highlighted misuse clusters, leading to prescribing restrictions in some regions. Close follow-up, documentation, urine screening and multidisciplinary care help detect problematic patterns early and coordinate interventions.
| Drug | Signal |
|---|---|
| Pregabalin | Higher misuse reports |
Cost Availability Insurance Coverage and Prescribing Advice
Brand-name pregabalin is often pricier than gabapentin, but generics have narrowed the gap. Out-of-pocket costs vary widely; capsule strengths, dosing frequency and pharmacy choice influence price. Mail-order and discount programs can reduce expenses for patients on long-term therapy. Patients should compare prices before filling and ask about manufacturer coupons.
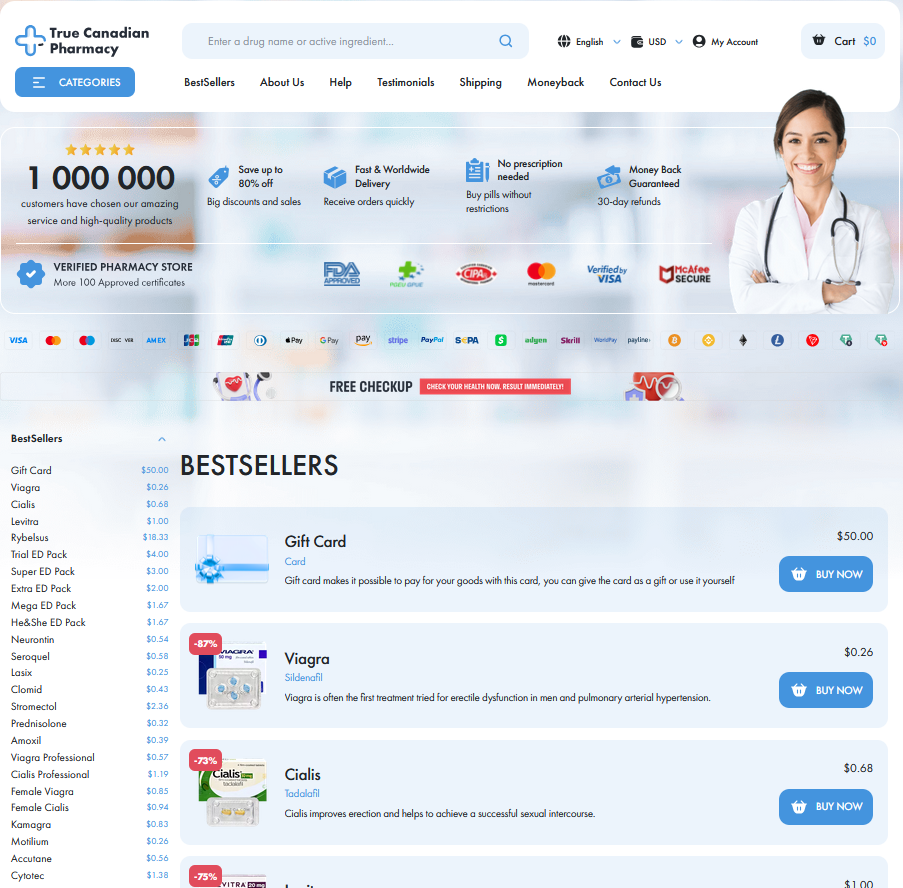
Formulary placement and prior authorization policies shape access, some insurers favor gabapentin as first-line due to lower cost, while others cover pregabalin for specific indications. Community pharmacies usually stock both, but rural shortages and supply-chain fluctuations occasionally disrupt supply. Telepharmacy and online pharmacies may offer alternatives but verify authenticity.
Clinicians should weigh efficacy, tolerability and patient resources when choosing between them, document rationale for nonpreferred options and discuss cost-saving strategies. Monitoring adherence, checking local formularies and revisiting therapy if cost barriers emerge improves outcomes and equity. And involve pharmacists early, regularly.

